Monitoring Landscape in Advanced Breast Cancer
Breast Cancer at a Glance1
- Breast cancer is the most common cancer and second leading cancer-related cause of death in women around the world, with an estimated 2.3 million diagnoses
- In 2022, breast cancer caused an estimated 670,000 deaths globally
- Roughly half of all breast cancers occur in women with no specific risk factors other than sex and age
- It was the most common cancer in women in 157 countries out of 185 in 2022
- Breast cancer occurs in every country in the world
- ~0.5–1% of breast cancers occur in men
What is Breast Cancer?
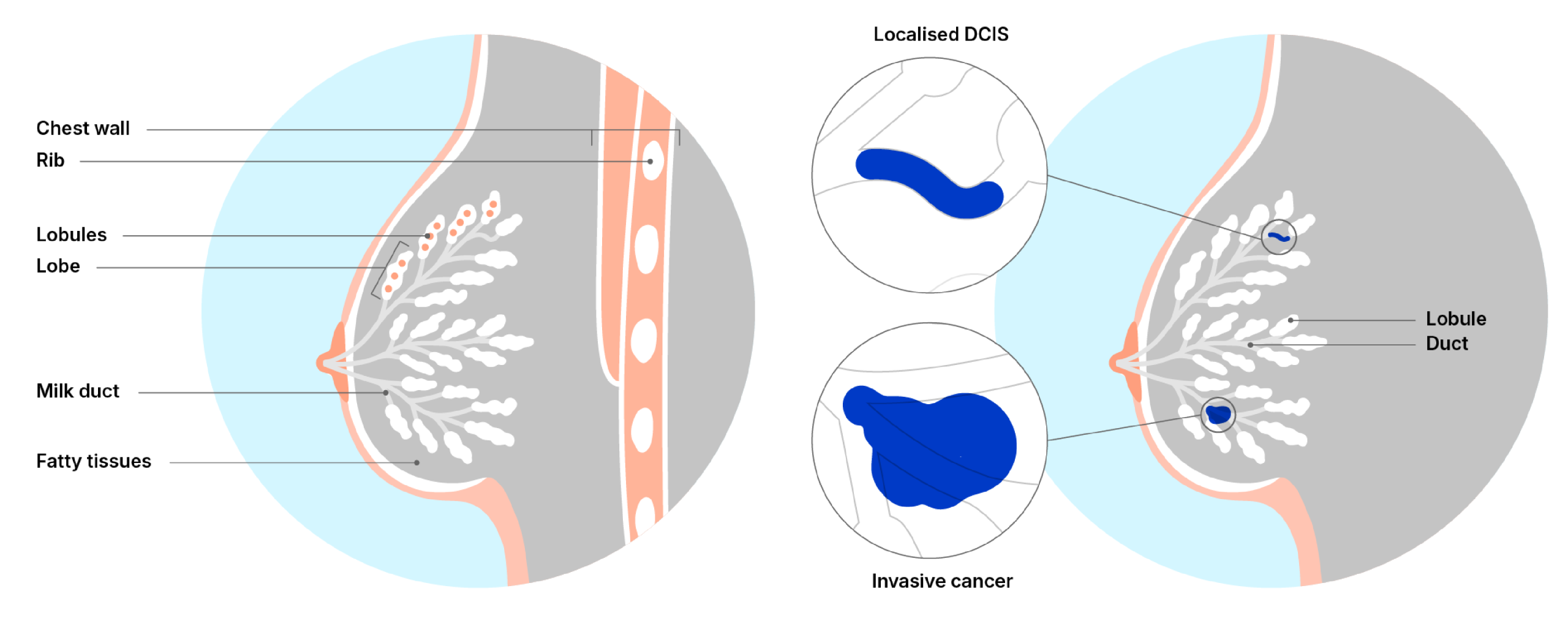
Breast cancer occurs when abnormal cells in the breast begin to grow and divide in an uncontrolled way and eventually form a tumour. Breast cancer most commonly starts in the cells that line the milk ducts of the breast.2
If the cells that turned cancerous are contained inside the ducts, this is classified as ductal carcinoma in situ (DCIS). However, if the cancerous cells have broken out of the duct and spread into the surrounding breast tissue, this is invasive breast cancer or invasive ductal carcinoma.2
Who is At Risk?
Being biologically female remains the most significant risk factor for developing breast cancer. Around 99% of patients diagnosed are women, with approximately 0.5–1% occurring in men. When breast cancer does occur in men, treatment approaches generally mirror those used for women.1
A variety of factors can elevate breast cancer risk, including increasing age, obesity, excessive alcohol consumption, family history of the disease, prior exposure to radiation, certain reproductive factors (such as age at first menstrual period and age at first pregnancy), tobacco use, and the administration of hormone therapy after menopause. Notably, about half of breast cancer cases arise in women with no clearly identifiable risk factors beyond being female and aged over 40.
While having a family history of breast cancer raises an individual’s risk, most women diagnosed do not report a known family history. Importantly, the absence of a known family history does not imply low risk.
Some inherited genetic mutations significantly increase the likelihood of developing breast cancer. The most impactful of these are mutations in the BRCA1, BRCA2, and PALB2 genes. Individuals carrying these high-risk variants may choose to pursue risk-reducing options such as preventive mastectomy and/or medication to lower risk.
Importance of Early Detection
Detecting breast cancer early greatly improves outcomes and reduces mortality. Early detection involves two key elements:1
- Screening: Using mammography to detect disease before symptoms appear, which is typically recommended for women aged 50–69 who do not have signs of breast cancer
- Early Diagnosis: Recognizing potential signs and symptoms, seeking medical evaluation promptly when abnormalities are noticed, and ensuring timely diagnosis and referral for treatment
How is Breast Cancer Treated?
Treatment for breast cancer depends on a number of factors. You might have a choice of treatments, or your medical team might recommend the best treatment for you. The main treatments for breast cancer include:3
- Surgery
- Hormone therapy (also called endocrine therapy)
- Chemotherapy
- Radiotherapy
- Targeted cancer drugs and immunotherapy
- Bone strengthening drugs (bisphosphonates)
Depending on your diagnosis, you may have a unique combination of these treatment options. This is why your treatment plan may be different from other people with breast cancer.
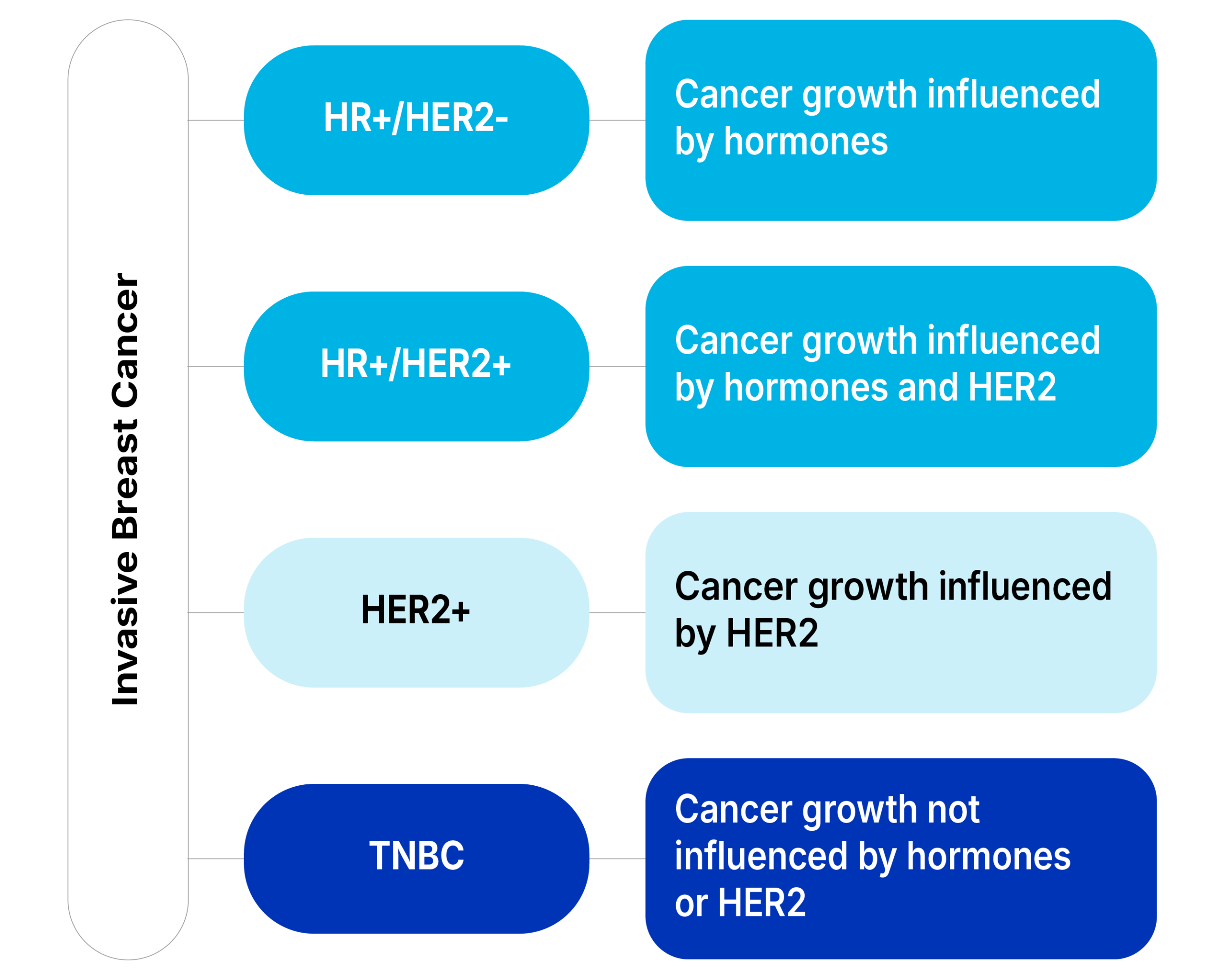
Breast Cancer Subtypes
Healthcare providers classify breast cancer subtypes by receptor cell status. Receptors are protein molecules in or on cells’ surfaces. They can attract or attach to certain substances in your blood, including hormones like estrogen and progesterone.
Estrogen and progesterone help cancerous cells grow. Finding out if cancerous cells have estrogen or progesterone receptors helps healthcare providers plan breast cancer treatment.
Subtypes include:4
- ER-positive (ER+) breast cancers have estrogen receptors
- PR-positive (PR+) breast cancers have progesterone receptors
- HR-positive (HR+) breast cancers have estrogen and progesterone receptors
- HR-negative (HR-) breast cancers don’t have estrogen or progesterone receptors
- HER2-positive (HER2+) breast cancers have higher than normal levels of the HER2 protein. This protein causes cancer cells to grow. About 15–20% of all breast cancers are HER2-positive
- Triple-negative (TNBC) breast cancers show no ER, PR or HER2 expression
Breast cancer is classified as HR+ when at least 1% of its cells show receptors for estrogen or progesterone.5 This means the tumor is influenced by these hormones and may respond well to therapies that block or reduce their effects. Hormone-based treatments, including tamoxifen and aromatase inhibitors (AI), work by disrupting the activity of estrogen and/or progesterone, which some cancer cells rely on for growth. Because of this hormone dependence, endocrine therapy is often one of the first treatment approaches for HR+ breast cancer.
View Available Treatments for HR+ Breast Cancer
Understanding Metastatic Breast Cancer
Nearly 30% of women diagnosed with early-stage breast cancer develop metastatic disease. Because there are so few cases of male breast cancer, it’s not clear how many of these breast cancers metastasize, but men are also diagnosed with metastatic breast cancer.
When the first diagnosis of breast cancer is metastatic, it is called de novo metastatic breast cancer. This means that the cancer has already spread to another part of the body and may be classified as stage IV breast cancer.
Metastatic breast cancer is made up of cells from the original tumor that developed in the breast. So if breast cancer spreads to the bone, the metastatic tumour in the bone is made up of breast cancer cells, not bone cancer cells. Common metastatic breast cancer signs and symptoms may include:
- back, joint or bone pain that does not go away
- difficulty urinating (either incontinence or not being able to go), which can be a sign that the cancer is pinching nerves in your back
- numbness or weakness anywhere in your body
- a constant dry cough
- shortness of breath or difficulty breathing
- chest pain
- loss of appetite
- abdominal bloating, pain, or tenderness
- constant nausea, vomiting
If the patient has a history of breast cancer and develops any of the above symptoms of metastatic breast cancer, one or more of the following tests may be recommended to see if the cancer has returned:6
- blood tests (including tumor markers in some patients)
- whole-body bone scan, with or without X-rays of specific bones
- MRI (magnetic resonance imaging) of the spine or brain
- CT (computed tomography) scan of the chest, abdomen, pelvis, or brain
- PET (positron emission tomography) scan
- X-ray or ultrasound of the abdomen or chest
- bronchoscopy, if you have a constant cough or trouble breathing
- biopsy of any suspicious area
There are a number of different approaches to treating metastatic breast cancer. Treatment plans focus on systemic therapies like hormone therapy (similar to early-stage breast cancer), chemotherapy, targeted therapy, and immunotherapy. Treatment decisions are based on where in the body the cancer has spread, the cancer’s characteristics (such as hormone receptor status and HER2 status), your symptoms, and any cancer treatments you’ve had in the past.
Conversely, physical symptoms, psychological stress and potential treatment side effects may heavily impact quality of life in patients with metastatic breast cancer. Treatment-related physical changes can also negatively affect self-perception emotional well-being.7
While some studies indicate that quality of life generally improves over time for most breast cancer patients post-treatment, others suggest that certain patients exhibit different quality of life trajectories, emphasizing the need for individualized interventions.7 However, variations in patient-doctor interactions and the potential consequences of over-informing patients may require tailored interventions based on the patients’ cultural background, societal norms and personal beliefs.
Monitoring Landscape in Advanced Breast Cancer
Breast Cancer at a Glance1
Breast cancer is the most common cancer and second leading cancer-related cause of death in women around the world, with an estimated 2.3 million diagnoses
In 2022, breast cancer caused an estimated 670,000 deaths globally
Roughly half of all breast cancers occur in women with no specific risk factors other than sex and age
It was the most common cancer in women in 157 countries out of 185 in 2022
Breast cancer occurs in every country in the world
~0.5–1% of breast cancers occur in men
What is Breast Cancer?
Breast cancer occurs when abnormal cells in the breast begin to grow and divide in an uncontrolled way and eventually form a tumour. Breast cancer most commonly starts in the cells that line the milk ducts of the breast.2
If the cells that turned cancerous are contained inside the ducts, this is classified as ductal carcinoma in situ (DCIS). However, if the cancerous cells have broken out of the duct and spread into the surrounding breast tissue, this is invasive breast cancer or invasive ductal carcinoma.2
Who is At Risk?
Being biologically female remains the most significant risk factor for developing breast cancer. Around 99% of patients diagnosed are women, with approximately 0.5–1% occurring in men. When breast cancer does occur in men, treatment approaches generally mirror those used for women.1
A variety of factors can elevate breast cancer risk, including increasing age, obesity, excessive alcohol consumption, family history of the disease, prior exposure to radiation, certain reproductive factors (such as age at first menstrual period and age at first pregnancy), tobacco use, and the administration of hormone therapy after menopause. Notably, about half of breast cancer cases arise in women with no clearly identifiable risk factors beyond being female and aged over 40.
While having a family history of breast cancer raises an individual’s risk, most women diagnosed do not report a known family history. Importantly, the absence of a known family history does not imply low risk.
Some inherited genetic mutations significantly increase the likelihood of developing breast cancer. The most impactful of these are mutations in the BRCA1, BRCA2, and PALB2 genes. Individuals carrying these high-risk variants may choose to pursue risk-reducing options such as preventive mastectomy and/or medication to lower risk.
Importance of Early Detection
Detecting breast cancer early greatly improves outcomes and reduces mortality. Early detection involves two key elements:1
Screening: Using mammography to detect disease before symptoms appear, which is typically recommended for women aged 50–69 who do not have signs of breast cancer
Early Diagnosis: Recognizing potential signs and symptoms, seeking medical evaluation promptly when abnormalities are noticed, and ensuring timely diagnosis and referral for treatment
How is Breast Cancer Treated?
Treatment for breast cancer depends on a number of factors. You might have a choice of treatments, or your medical team might recommend the best treatment for you. The main treatments for breast cancer include:3
Surgery
Hormone therapy (also called endocrine therapy)
Chemotherapy
Radiotherapy
Targeted cancer drugs and immunotherapy
Bone strengthening drugs (bisphosphonates)
Depending on your diagnosis, you may have a unique combination of these treatment options. This is why your treatment plan may be different from other people with breast cancer.
Breast Cancer Subtypes
Healthcare providers classify breast cancer subtypes by receptor cell status. Receptors are protein molecules in or on cells’ surfaces. They can attract or attach to certain substances in your blood, including hormones like estrogen and progesterone.
Estrogen and progesterone help cancerous cells grow. Finding out if cancerous cells have estrogen or progesterone receptors helps healthcare providers plan breast cancer treatment.
Subtypes include:4
ER-positive (ER+) breast cancers have estrogen receptors
PR-positive (PR+) breast cancers have progesterone receptors
HR-positive (HR+) breast cancers have estrogen and progesterone receptors
HR-negative (HR-) breast cancers don’t have estrogen or progesterone receptors
HER2-positive (HER2+) breast cancers have higher than normal levels of the HER2 protein. This protein causes cancer cells to grow. About 15–20% of all breast cancers are HER2-positive
Triple-negative (TNBC) breast cancers show no ER, PR or HER2 expression
Breast cancer is classified as HR+ when at least 1% of its cells show receptors for estrogen or progesterone.5 This means the tumor is influenced by these hormones and may respond well to therapies that block or reduce their effects. Hormone-based treatments, including tamoxifen and aromatase inhibitors (AI), work by disrupting the activity of estrogen and/or progesterone, which some cancer cells rely on for growth. Because of this hormone dependence, endocrine therapy is often one of the first treatment approaches for HR+ breast cancer.
View Available Treatments for HR+ Breast Cancer
Understanding Metastatic Breast Cancer
Nearly 30% of women diagnosed with early-stage breast cancer develop metastatic disease. Because there are so few cases of male breast cancer, it’s not clear how many of these breast cancers metastasize, but men are also diagnosed with metastatic breast cancer.
When the first diagnosis of breast cancer is metastatic, it is called de novo metastatic breast cancer. This means that the cancer has already spread to another part of the body and may be classified as stage IV breast cancer.
Metastatic breast cancer is made up of cells from the original tumor that developed in the breast. So if breast cancer spreads to the bone, the metastatic tumour in the bone is made up of breast cancer cells, not bone cancer cells. Common metastatic breast cancer signs and symptoms may include:
back, joint or bone pain that does not go away
difficulty urinating (either incontinence or not being able to go), which can be a sign that the cancer is pinching nerves in your back
numbness or weakness anywhere in your body
a constant dry cough
shortness of breath or difficulty breathing
chest pain
loss of appetite
abdominal bloating, pain, or tenderness
constant nausea, vomiting
If the patient has a history of breast cancer and develops any of the above symptoms of metastatic breast cancer, one or more of the following tests may be recommended to see if the cancer has returned:6
blood tests (including tumor markers in some patients)
whole-body bone scan, with or without X-rays of specific bones
MRI (magnetic resonance imaging) of the spine or brain
CT (computed tomography) scan of the chest, abdomen, pelvis, or brain
PET (positron emission tomography) scan
X-ray or ultrasound of the abdomen or chest
bronchoscopy, if you have a constant cough or trouble breathing
biopsy of any suspicious area
There are a number of different approaches to treating metastatic breast cancer. Treatment plans focus on systemic therapies like hormone therapy (similar to early-stage breast cancer), chemotherapy, targeted therapy, and immunotherapy. Treatment decisions are based on where in the body the cancer has spread, the cancer’s characteristics (such as hormone receptor status and HER2 status), your symptoms, and any cancer treatments you’ve had in the past.
Conversely, physical symptoms, psychological stress and potential treatment side effects may heavily impact quality of life in patients with metastatic breast cancer. Treatment-related physical changes can also negatively affect self-perception emotional well-being.7
While some studies indicate that quality of life generally improves over time for most breast cancer patients post-treatment, others suggest that certain patients exhibit different quality of life trajectories, emphasizing the need for individualized interventions.7 However, variations in patient-doctor interactions and the potential consequences of over-informing patients may require tailored interventions based on the patients’ cultural background, societal norms and personal beliefs.